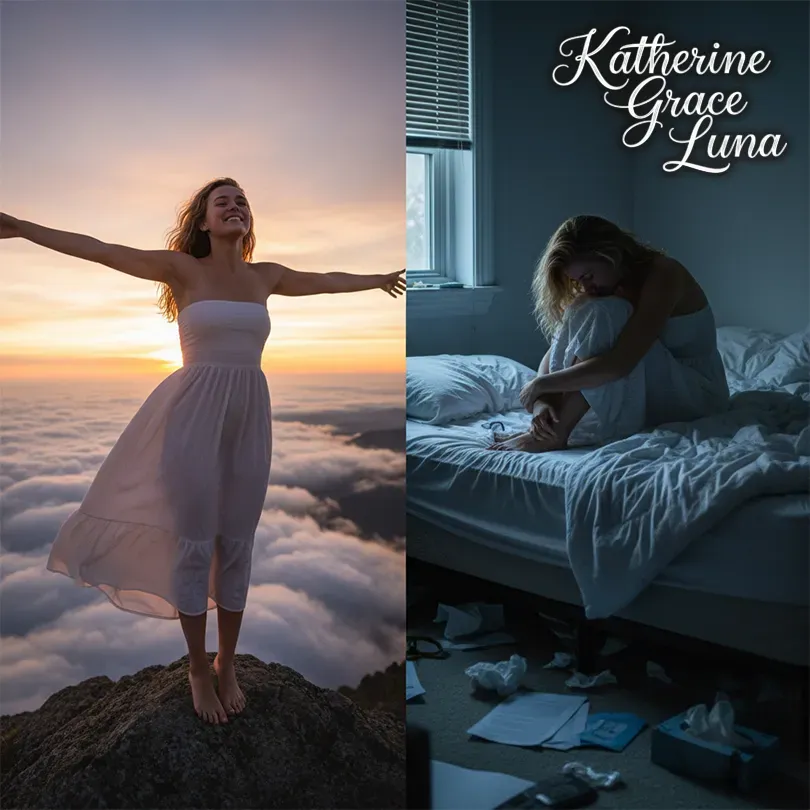
Morning Highs, Evening Lows? When Mood Swings Cross the Line Into Bipolar Disorder

Ever felt like you're on top of the world one day, then struggling to get out of bed the next? While we all experience emotional ups and downs, for some people, these mood swings are far more intense than typical daily fluctuations. When these extremes start disrupting your life, it might be time to consider whether you're dealing with bipolar disorder.
Understanding Bipolar Disorder: More Than Just Mood Swings
Bipolar disorder affects approximately 2.8% of U.S. adults – that's about 7 million people navigating life with this condition. Despite what many think, it's not simply being "moody" or "emotional." It's a serious mental health condition characterized by extreme shifts in mood, energy, and activity levels that can significantly impact daily functioning.
The average age of onset is around 25 years old, though symptoms can appear in teens or even later in life. What's particularly concerning is that it often takes up to 10 years from the first symptoms to receive an accurate diagnosis. That's a decade of confusion, misdiagnosis, and potentially inadequate treatment.
The Two Main Types: Similar Names, Different Experiences
Bipolar I Disorder: The Full Spectrum
To be diagnosed with Bipolar I, you need to have experienced at least one manic episode lasting 7 days or more (or severe enough to require hospitalization). These manic episodes aren't just feeling really happy or productive. We're talking about:
- Feeling invincible or having grandiose ideas about your abilities
- Needing only 2-3 hours of sleep and feeling completely rested
- Talking so fast others can't keep up
- Starting multiple ambitious projects simultaneously
- Making risky decisions like spending sprees, impulsive investments, or dangerous activities
- Sometimes experiencing psychotic symptoms like hallucinations or delusions
You don't necessarily need to experience depression to have Bipolar I, though about 70% of people do have depressive episodes as well.

Bipolar II Disorder: The Misunderstood Sibling
Bipolar II requires at least one hypomanic episode (4+ days) AND one major depressive episode. Hypomania is like mania's quieter cousin – you might feel unusually productive, creative, or social, but it doesn't completely derail your life.
Here's the catch: many people with Bipolar II actually enjoy their hypomanic episodes. You're getting things done, you're charismatic, you're the life of the party. It's the crushing depressive episodes that usually drive people to seek help, which is why Bipolar II is often misdiagnosed as major depression.
The depressive episodes in Bipolar II can actually be more frequent and longer-lasting than in Bipolar I, making it equally challenging despite the absence of full mania.
How Do You Know It's Not Just Regular Mood Changes?
Everyone has good days and bad days. The difference with bipolar disorder is like comparing gentle waves to a tsunami. Normal mood fluctuations are manageable – you might feel sad about something specific, then gradually feel better. You maintain control.
With bipolar episodes:
- Emotions feel overwhelming and uncontrollable
- Episodes last for distinct periods (days to weeks)
- There's significant impairment in work, relationships, or daily activities
- The changes are noticeable to others
- You might not even recognize you're in an episode until it's over
The Reality of Living with Bipolar Disorder
The statistics paint a sobering picture. People with bipolar disorder face:
- 9-13 years reduction in life expectancy
- 10-30 times higher risk of suicide compared to the general population
- Increased risk of cardiovascular disease and metabolic disorders
- High rates of co-occurring conditions like anxiety disorders and substance use
But here's the crucial part: with proper treatment, people with bipolar disorder can lead fulfilling, productive lives.

Treatment That Actually Works
The good news? Treatment success rates are encouraging. Modern approaches combine:
Medication Management:
- Mood stabilizers like lithium (still the gold standard after 70+ years)
- Anticonvulsants for mood stabilization
- Antipsychotics for acute episodes
- Careful use of antidepressants (only with mood stabilizers to prevent triggering mania)
Psychotherapy:
- Cognitive Behavioral Therapy (CBT) to identify triggers and manage symptoms
- Interpersonal therapy to improve relationships
- Psychoeducation to understand the condition
- Family therapy to build support systems
Lifestyle Modifications:
- Regular sleep schedules (crucial for mood stability)
- Exercise and stress management
- Mood tracking to identify patterns
- Avoiding alcohol and drugs
Studies show that people who engage with support groups have 86% better treatment compliance and significantly reduced hospitalizations.
Why Early Recognition Matters
If you're in your early 20s and noticing extreme mood patterns, pay attention. The earlier you get proper treatment, the better your long-term outcomes. Many people spend years being treated for depression alone, when they actually have bipolar disorder – leading to inadequate treatment and potentially worsening symptoms.
Red flags to watch for:
- Periods of unusually high energy and productivity
- Decreased need for sleep without feeling tired
- Rapid speech or racing thoughts
- Impulsive decisions you later regret
- Severe depression that doesn't respond well to antidepressants alone
- Family history of bipolar disorder or severe mood disorders
The Bottom Line
Bipolar disorder isn't a character flaw or a sign of weakness. It's a medical condition that affects the brain's ability to regulate mood – and it's highly treatable. If you recognize these patterns in yourself or someone you care about, reaching out to a mental health professional isn't just important, it could be life-changing.
Remember, that friend who seems to swing between being the life of the party and disappearing for weeks? That colleague who has bursts of incredible productivity followed by calling in sick for days? They might be dealing with more than just personality quirks. Understanding bipolar disorder helps us support each other better and reduces the stigma that keeps people from seeking help.
The path from recognition to recovery isn't always straightforward, but with the right support and treatment, stability is absolutely achievable. And that's something worth working toward.
